CALORIES
Trial of the route of early nutritional support in critically ill adults
Harvey SE, Parrott F, Harrison DA, et al.; CALORIES Trial Investigators.
N Engl J Med. 2014 Oct 30;371(18):1673-84. [Full Text]
The timing and route of delivery of nutrition in the critically ill patient remains a complex decision, but most agree that some form of nutrition should be considered as early as possible. The enteral route has long been preferred but many factors, rightly or not, limit its use in practice: namely, need of and malfunctioning of feeding tubes, aspiration concerns, high gastric residual volumes (which are not reflective of actual motility), concerns while receiving high doses of vasopressors, or just prioritizing other aspects of ICU care [2]. The parenteral route, though more invasive, may be more “reliable but is associated with infection and had been associated with greater risks and complications [1].
The authors noted that prior “studies have not considered improvements in delivery, formulation, and monitoring of parenteral nutrition”. The authors cite a meta-analysis of 9 trials with intention-to-treat analyses that found a benefit to parenteral nutrition (odds ratio, 0.51; 95% CI, 0.27 to 0.97) [1,2]. They hypothesized that the parenteral route was superior to the enteral route for the delivery of early nutritional support in adults which was assessed in the CALORIES trial
Population
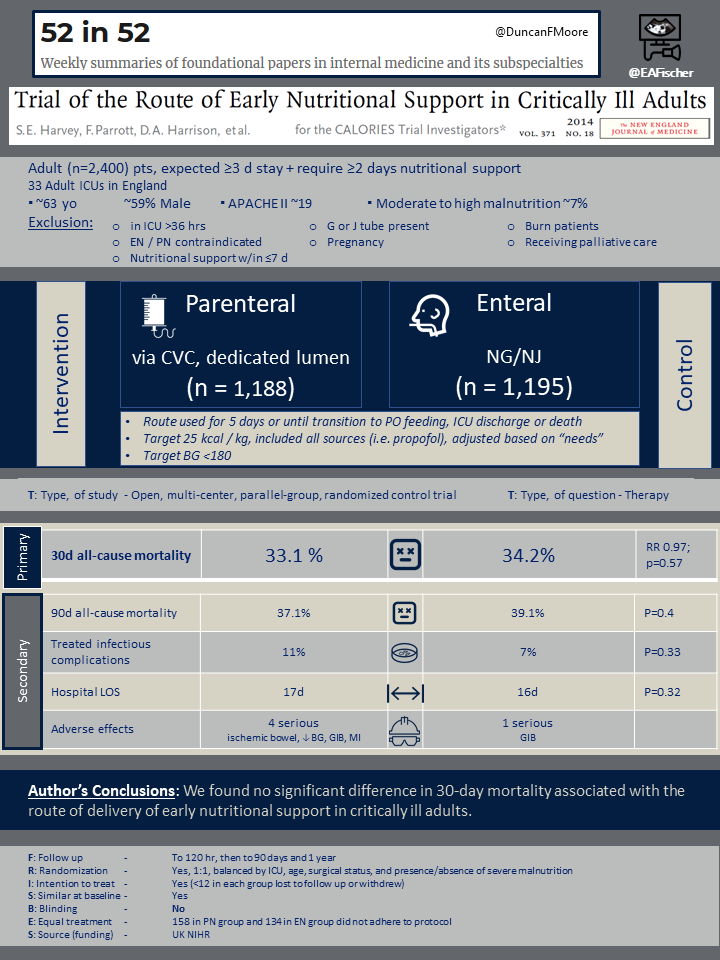
A total of 2,400 patients were enrolled from 33 Adult ICUs in England. Eligible patients were expected to have an ICU stay ≥3 days and to require ≥2 days of nutritional support.
Patients were excluded if they had already been in the ICU for >36 hours, enteral nutrition (EN) or parenteral nutrition (PN) were contraindicated, they had received nutritional support within the last 7 days, they had an existing G or J tube, were pregnant, a burn patient or were receiving palliative care.
The average age was ~63 years, most patients were male (~59%), the average APACHE II was ~19 and only the minority (~7%) had moderate to high malnutrition on enrollment.
Design
Patients were randomized in a 1:1 fashion and allocation was balanced by ICU, age, surgical status, and presence/absence of severe malnutrition. Patients either received PN via a central line with a dedicated lumen or EN via an NG or NJ, either of which was initiated within the first 36 hours. This route was to be used exclusively for 5 days or until transition to exclusive oral feeding, discharge from the ICU, or death. The target goal was 25 kcal / kg, which was to include all caloric sources (i.e. propofol), and could be further adjusted based on individual patient needs. Follow up was planned out to 1 year, with data gathered within the frist 120 hr, then to 90 days and finally to 1 year.
Results
Of the 2,400 enrolled, 1,188 patients were allocated to the PN group and 1,195 to the EN group. Less than 12 in each group were lost to followup but 158 in PN group and 134 in EN group did not adhere to protocol or had crossover, but were still included in the intention to treat analysis
The primary endpoint was 30 day all-cause mortality and there was no difference between the PN and EN groups (33.1% vs. 34.2%; RR 0.97; p=0.57). There were multiple important secondary outcomes. There was no difference in 90 day all-cause mortality (37.1% vs. 39.1%; RR 0.96; p=0.4), duration of organ support, infectious complications (22% vs. 21%, p=0. 72), or ICU (8.1 d vs. 16 d, p=0.15) and hospital LOS (17 d vs. 16 d, p=0.32).
Rates of adverse effects were similar in each group (4.9% vs. 4.8%,p=1). There were only 4 serious AEs in the PN group (ischemic bowel, hypoglycemia, GIB, MI) and 1 in the EN group.
Discussion
CALORIES was a well designed study with good follow-up. While it was open-label, it was pragmatic, reflecting real practice. Prior evidence had suggested PN may have an advantage to EN in this population but ultimately no benefit was demonstrated.
Many commonly held advantages of either the PN or EN route were not supported by results in this study. One reason PN was purported to have an advantage was that calories could be more reliably delivered. Interestingly, neither group met caloric goals (21.3 kcal/kg vs. 18.5 kcal/kg). Additionally, there were not more infections in the PN group, a risk often cited. Conversely, while EN was associated with vomiting, infections were also low, possibly from better aspiration prevention and VAP precautions, and hypoglycemia episodes had no measured clinical impact.
Currently ASPEN guidelines from 2016 continue to recommend “EN over PN in critically ill patients who require nutrition support therapy”, and that the EN “be initiated within 24–48 hours” if the patient “is unable to maintain volitional intake“, though the evidence quality is noted as very low to low for each. CALORIES may not have shown that early PN has additional benefit but it did suggest traditional PN risks were low. Prior iterations of ASPEN guidelines were hesitant to recommend early PN if EN was not feasible. Now, PN initiation is recommended as soon as possible following ICU admission, if an ICU pt is at high nutrition risk (e.g. NUTRIC score ≥5) or is severely malnourished and EN is not feasible [3].
- Harvey SE, Parrott F, Harrison DA, et al.; CALORIES Trial Investigators. Trial of the route of early nutritional support in critically ill adults. N Engl J Med. 2014 Oct 30;371(18):1673-84.
- Cook D, Arabi Y. The route of early nutrition in critical illness. N Engl J Med. 2014 Oct 30;371(18):1748-9.
- McClave SA, Taylor BE, Martindale RG, et al. ; Society of Critical Care Medicine; American Society for Parenteral and Enteral Nutrition. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr. 2016 Feb;40(2):159-211.
