Mars Cosmonaut Salt Study – Effect of Long Term Sodium Intake
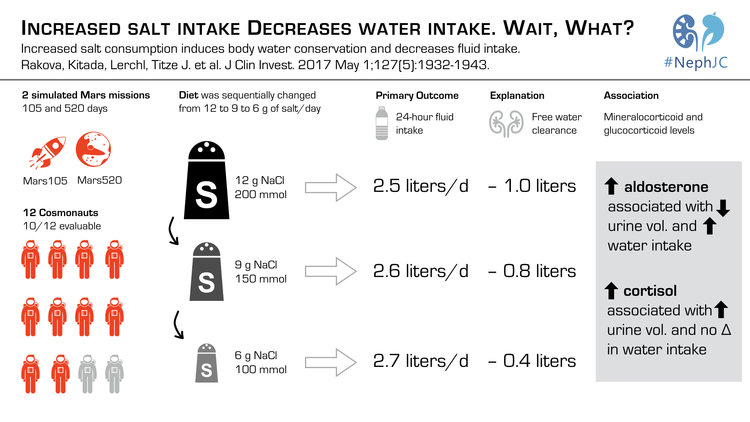
Increased Salt Consumption Induces Body Water Conservation and Decreases Fluid Intake.
Rakova N, Kitada K, Lerchl K, et al.
J Clin Invest. 2017 May 1;127(5):1932-1943. [Full text]
NY Times take
The common understanding of the relationship between salt and fluid intake is both simple – that sodium intake stimulates thirst, which stimulates fluid intake – as well as central to explaining how osmotic balance is maintained. But like everything in physiology it is more complex and still being elucidated.
In medicine we often consider the sodium (Na) in plasma. But a large portion of the total body Na is in the bone, cartilage, and connective tissue, like skin [1, 2]. The existence of a Na reservoir suggests that Na homeostasis is not maintained purely at the level of the nephron. Prior work suggests that the is a cyclic hormonal control to Na homeostasis, in weekly or monthly cycles, the length of which seem to be influenced by total Na intake [3].
The current study took advantage of two prolonged space simulations in which dietary intake was regulated.
Patient population and Design
Participants were simulating acting and living as cosmonauts on the International Space Station. Two separate simulations, of 105 (Mars105) and 520 (Mars520) days each, were part of the study. Participants lived for these periods in a hermatically sealed environment with controlled intake of non sodium containing minerals and calories. Fluid intake was unrestricted. The controlled variable was Na intake.
In Mars 105, salt intake was adjusted about every 29 days from 12 g / d (12 g NaCl = 4.6 g Na = 200 mEq Na), to 9 g/d (150 mEq) then finally to 6 g/d (100 mEq Na) with . Mar520, which was only monitored through day 205 had a similar progression from 12 to 6 g/d, but then returned to 12 g/d.
The participants measured and recorded their fluid intake as well as collected 24-hour urine samples. There were 12 participants initially but only the 10 participants that had very accurate recording of intake and output were included in the analysis.
The effects of varied Na intake on daily water intake and urine volume, urinary Na, cortisone, and aldosterone excretion; urine Na+, K+, and urea concentration; and urine osmolality were all tracked.
Results
The authors found that, as expected, as dietary Na increased, so did the average daily urinary Na . But what was a surprise was that the same increase in dietary Na led to decreased fluid intake even though urinary volume increased! (Figure 1)
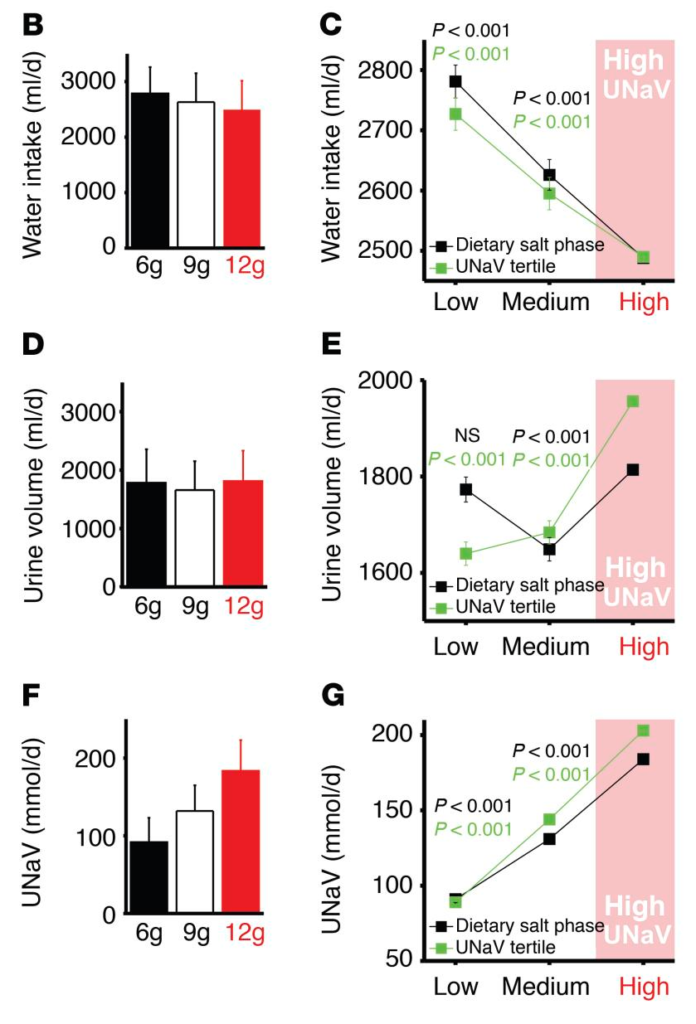
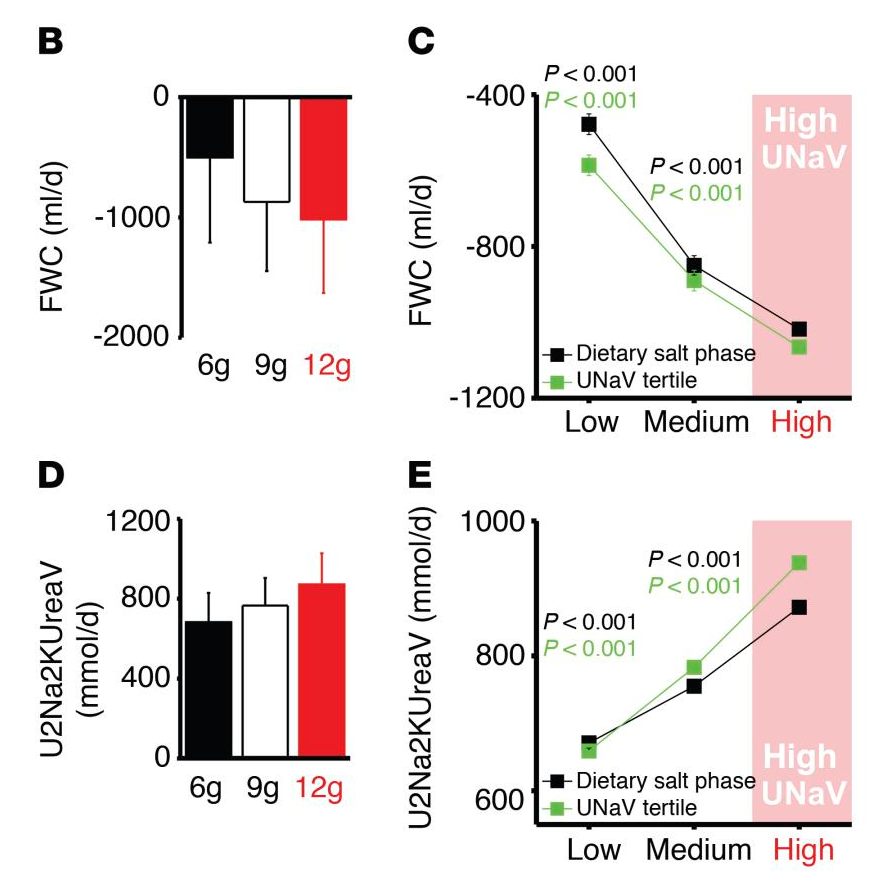
Na homeostasis seemed to be achieved not by more water intake, but more free water generation in the kidney with more Na intake, leading to less free water clearance (Figure 2).
Na intake did have some effect on aldosterone but mostly urinary aldosterone and cortisol had rhythmic half-weekly and weekly patterns of change that were largely independent of salt intake. At the 6-g/d Na intake level there was some reduction in rhythmic aldosterone and enhancement of rhythmic glucocorticoid action.
The authors found that higher aldosterone was associated with less urine volume and more water intake (total body water increased) while more cortisol was associated with increased urine volume without increased water intake.
Discussion
The nuances of the findings of this study are far reaching and complex. And perhaps more questions are generated than answered. But the study challenges the notion that higher Na intake triggers thirst and increases water intake, at least over the long term. Also, that Na intake was not immediately coupled with matching Na output was also a surprise.
How then is homeostasis achieved? The authors purport that cyclic aldosterone and cortisone lead to variable free water retention and excretion that are independent of Na intake. These hormonal changes allows for a free water reservoir that can adapt to higher sodium intake. Additionally, the kidney, more so than a thirst response, serves as “a biological barrier designed for water conservation… [and] separates osmolytes from water to prevent dehydration while conducting osmolyte balance”.
This is a small study, and one whose conditions will be hard to replicate or extrapolate to the real world. Regardless, its implications may be as simple as rethinking a 24 hour urine collection (maybe collections need to be weekly or monthly to account for rhythmic variations?). Or the findings may influence dietary or fluid intake recommendations, especially as Na intake does have some effect on activity of aldosterone and cortisone.
| F: Follow up | 105 to 205 days |
| R: Randomization | NO |
| I: Intention to treat | NO |
| S: Similar at baseline | Yes |
| B: Blinding | NO |
| E: Equal treatment | Yes |
| S: Source (funding) | Federal Ministry for Economics and Technology/DLR; the Interdisciplinary Centre for Clinical Research; the NIH; the American Heart Association (AHA); the Renal Research Institute; and the TOYOBO Biotechnology Foundation |
- Sterns RH. Disorders of plasma sodium. N Engl J Med. 2015 Mar 26;372(13):1269.
- NephJC Chat, Increased salt consumption induces body water conservation and decreases fluid intake. nephjc.com
- Rakova N, Jüttner K, Dahlmann A, et al. Long-term space flight simulation reveals infradian rhythmicity in human Na(+) balance. Cell Metab. 2013 Jan 8;17(1):125-31.