TTM2 – Hypothermia versus Normothermia for Cardiac Arrest
Hypothermia versus Normothermia after Out-of-Hospital Cardiac Arrest.
Dankiewicz J, Cronberg T, Lilja G, et al; TTM2 Trial Investigators.
N Engl J Med. 2021 Jun 17;384(24):2283-2294. [Full text]
Hypothermia theoretically decreases cerebral oxygen demands, and hence was postulated to minimize ischemia post cardiac arrest. Two small trials (HACA, n=137 [1]and Bernard trials, n=77 [2]) were simultaneously published in 2002 that became the foundation for which hypothermia was adopted. But these small trials had methodological limitations such as missing data, high risk for selection bias, worse control of fever and less staff attention in the control group to name a few (explored further by @emcrit and @first10em).
By 2013 hypothermia protocols were in common use and the TTM1 trial of 950 patients established that “33°C did not confer a benefit as compared with a targeted temperature of 36°C” [3]. As Josh Farkas argues that hypothermia had become the standard and status quo bias prevented many from moving merely to normothermia.
Given the benefit of hypothermia remained in guidelines even if based on, per the TTM2 authors, data of “low certainty”, these investigators sought to assess whether hypothermia truly offered a mortality benefit compared to simply preventing fever.
Design and Patients
This was an international, multi-center, parallel group representing 14 countries and 61 institutions.The clinical teams were not blinded however all adjudicators of data and outcomes were blinded.
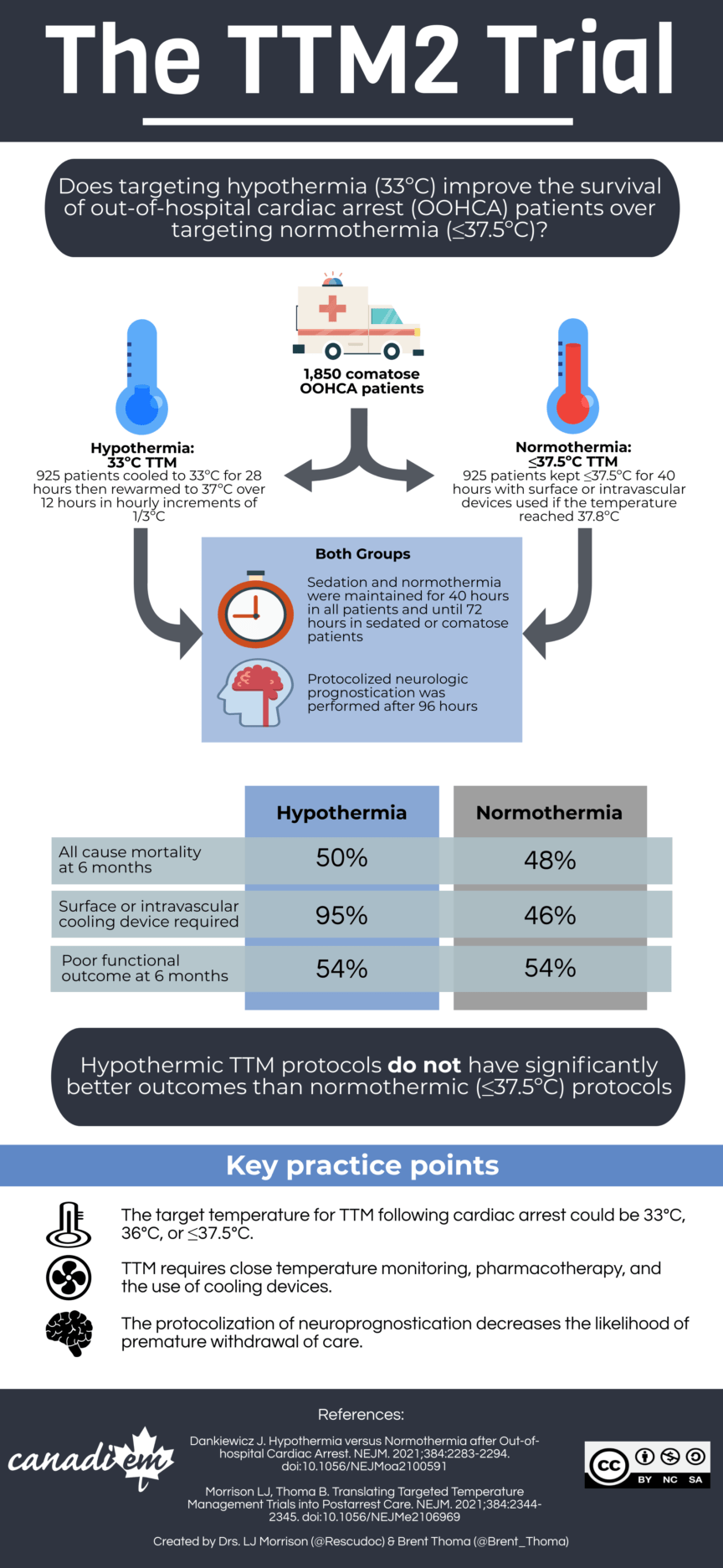
Consecutively screened adults (≥18 years) were included if they had an out-of-hospital cardiac arrest, presumed or confirmed and had sustained ROSC >20 minutes but enrolled no later than 180 minutes after ROSC, and remained unconscious (FOUR score motor response <4), not able to obey commands or respond verbally to pain.
Patients were excluded if the arrest was unwitnessed and the initial rhythm was asystole. They could not have a temperature on admission < 30°C or be on ECMO prior to ROSC.
A total of 4355 patients were screened, and 55% did not meet inclusion criteria. 1861 were analyzed as intention to treat, 930 in Hypothermia arm and 931 in Normothermia arm and 1850 were analyzed for survival (as 11 were lost to follow-up).
Intervention and Outcomes
In the normothermia group, the aim was to maintain a temperature of ≤37.5°C with conservative and pharmacologic measures. If those failed (temperature reached ≥37.8°C) cooling with a surface or intravascular temperature-management device was initiated with a target temperature of 37.5°C. No active warming or cooling was provided otherwise below 37.8°C.
The primary outcome was death from any cause at 6 months. The main pre-specified secondary outcome wasa poor functional outcome at 6 months, defined as a score of 4 to 6 on the modified Rankin scale.
Results
The average age was 64 yrs, ~90% were male and most had a shockable rhythm (72-75%, mostly v-fib). STEMI was present in ~40%.
There was no difference in all-cause mortality at 6 months, with 50% mortality in the hypothermia group and 48% in the normothermia, RR 1.04 (95% CI 0.94-1.14, p = 0.37). The functional outcomes were similar as well, 55% poor in bothe groups, RR 1.0 (95% CI 0.92–1.09).
Patients in the hypothermia group experienced unexpected severe adverse events (3.7% vs. 1.4%, p=0.003) and arrhythmias that resulted in hemodynamic compromise more common in the hypothermia group., 24% vs. 16%, RR 1.45 (95% CI 1.21–1.75, p = <0.001). Additionally patients in the hypothermia group required more paralytics (66% vs. 45%, p<0.001), had a longer median length of mechanical ventilation (3.8 days vs. 2.9 days).
Discussion
This was a large well designed study that sought to assess whether hypothermia truly offered a mortality benefit compared to simply preventing fever. Methodological concerns of early trials are absent here: blinding wherever possible, intention to treat, < 1% missing data on mortality, only 3 protocol deviations related to temperature management.
Between TTM2 and meta-analysis of prior trials [4], there does not appear to be a role for hypothermia in Out-of-Hospital Cardiac Arrest. For In-Hospital-Cardiac-Arrest it remains an unanswered question. Two studies have demonstrated no benefit from hypothermia for traumatic brain injury (POLAR and EUROTHERM). But it may be simply that hypothermia’s theoretical benefits were just theoretical.
| F: Follow up | 24 mo (30 days, 6 months, 24 months, ongoing) |
| R: Randomization | Yes, stratified by site and trial (2 trials combined in 1) |
| I: Intention to treat | Yes |
| S: Similar at baseline | Yes |
| B: Blinding | Clinicians non-blinded. All assessors (of prognosis, participants, outcome) and statisticians and data managers were blinded. |
| E: Equal treatment | Yes |
| S: Source (funding) | Swedish Research Council and others |
- Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002 Feb 21;346(8):549-56.
- Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, Smith K. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002 Feb 21;346(8):557-63.
- Nielsen N, Wetterslev J, Cronberg T, et al.; TTM Trial Investigators. Targeted temperature management at 33°C versus 36°C after cardiac arrest. N Engl J Med. 2013 Dec 5;369(23):2197-206.
- Kim JH, Nagy Á, Putzu A, Belletti A, Biondi-Zoccai G, Likhvantsev VV, Yavorovskiy AG, Landoni G. Therapeutic Hypothermia in Critically Ill Patients: A Systematic Review and Meta-Analysis of High Quality Randomized Trials. Crit Care Med. 2020 Jul;48(7):1047-1054.