CABANA – 5 year Recurrence
Recurrence of Atrial Fibrillation After Catheter Ablation or Antiarrhythmic Drug Therapy in the CABANA Trial.
Poole JE, Bahnson TD, Monahan KH, et al.; CABANA Investigators and ECG Rhythm Core Lab.
J Am Coll Cardiol. 2020 Jun 30;75(25):3105-3118. [Full Text]
Summary by Elizabeth Bierbower, MD
Atrial fibrillation (AF) is the the most common cardiac tachyarrhythmia and is associated with an increased risk of mortality, stroke, heart failure, and peripheral embolism. AF occurs in approximately 6% of individuals greater than 65 and increases in prevalence with age, affecting 10% of individuals older than 80.
This study sought to determine if the management of AF with catheter ablation was more effective than antiarrhythmic drug therapy in reducing the recurrence of AF. As catheter ablation of atrial fibrillation has evolved over the past several decades as a valuable first-line treatment option for patients with AF this question has gained increasing importance.
The results from the study demonstrated that when compared to antiarrhythmic drug therapy, catheter ablation significantly reduces the recurrence of symptomatic and asymptomatic atrial fibrillation.
Patient population
Patients enrolled in the CABANA trial included patients that had symptomatic atrial fibrillation and were either older than 65 years of age or younger than 65 years with 1 or more major risk factors for stroke.
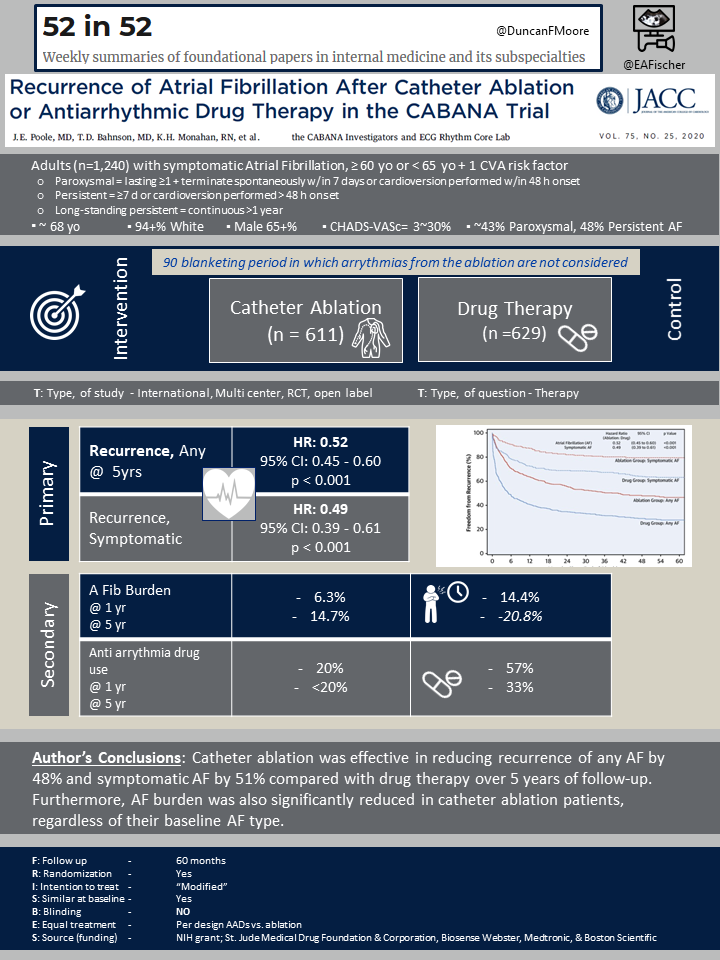
Initially 2,204 patients were enrolled in the original CABANA trial. Importantly that analysis found that catheter ablation, compared with medical therapy, did not significantly reduce the primary composite end point of death, disabling stroke, serious bleeding, or cardiac arrest. However, the question of disease burden and AF recurrence was part of the secondary analysis and ablation did reduce AF recurrence (HR, 0.52 [95% CI, 0.45-0.60]; P < .001).
This is an expanded analysis on the original CABANA population. It was conducted on 1,240 patients that were monitored for recurrent AF using the specific ECG recording monitor system provided by the CABANA trial. Patients originally included in the CABANA trial who were at sites unable to use the CABANA ECG recording monitor or who declined to use them were excluded.
Of 1,240 patients, the median age was 68 years, 34.4% were women, and 6.0% were African American or belonged to other nonwhite racial groups. The baseline pattern of AF was paroxysmal in 43.0% and persistent or long-standing persistent in 57.0%.
Outcomes
The study was conducted in order to evaluate the recurrence of atrial fibrillation in those that underwent catheter ablation compared to antiarrhythmic drug therapy with the primary outcome of symptomatic and asymptomatic atrial fibrillation recurrence. Major secondary outcomes included atrial fibrillation burden. Adverse safety events associated with the ablation procedure were rare. Pericardial effusion with tamponade was the most commonly reported adverse event in the ablation population.
Results
The patients randomized to the ablation group compared to the antiarrhythmic drug group had similar baseline demographics and clinical characteristics. The average age was 68 years and the majority of study participants were white men.
A modified intention-to-treat analysis was performed using a Cox proportional hazards model (adjusted for age at enrollment, ethnicity, AF type (paroxysmal, persistent, or long-standing persistent), years since onset of AF, history of congestive heart failure, structural heart disease, CHA2DS2-VASc score, history of coronary artery disease, and hypertension. Catheter ablation was associated with a significant reduction in any recurrence of AF (HR: 0.52; 95% CI: 0.45 to 0.60; p < 0.001) and a significant reduction in recurrence of symptomatic AF (HR: 0.49; 95% CI: 0.39 to 0.61; p < 0.001).
At 5 years, the ablation group experienced atrial fibrillation 14.7% of recorded Holter time compared to and 20.8% in the drug group.
Discussion
Atrial fibrillation is a common arrhythmia that affects a large portion of the population. AF is associated with significant morbidity and mortality, leading to increased incidence of stroke, heart failure, and death. This study demonstrated that catheter ablation for atrial fibrillation significantly lowers the rate of recurrence compared to medical therapy. Additionally, this study demonstrated that catheter ablation reduces the burden of AF following catheter ablation.
The CABANA study found that catheter ablation had a non-significant 14% reduction in death, disabling stroke, serious bleeding, or cardiac arrest. The CASTLE-AF trial more specifically studied ablation for AF in patients with heart failure and demonstrated a significantly lower rate of death from any cause or hospitalization following ablation compared to medical therapy.
This study indicates that ablation therapy, while perhaps has not been shown to clearly impact mortality or other serious morbidity, has a role in the disease burden and preventing recurrence. Therefore, referring physicians should understand that while ablation has an important role in the management of AF, the decision to pursue an invasive procedure requires discussion of the true proven benefits and that shared decision making is key.
