Timing of ERCP in Acute Cholangitis
Outcomes Associated With Timing of ERCP in Acute Cholangitis Secondary to Choledocholithiasis.
Parikh MP, Wadhwa V, Thota PN, Lopez R, Sanaka MR.
J Clin Gastroenterol. 2018 Nov/Dec;52(10):e97-e102. [Full Text]
Ascending cholangitis occurs when there is an obstruction to the biliary tree and can lead to bacteremia and sepsis secondary to elevated biliary pressures and must be managed as a medical emergency. Approximately 50% of ascending cholangitis are due to choledocholithiasis. The most predominant organisms are E. coli (22%), Klebsiella (18%) and enterococcus (15%) [1]. Based off the Tokyo guidelines, acute cholangitis can be divided into three grades. Grade III (severe) is defined as acute cholangitis with at least one organ system dysfunction: hypotension requiring pressors, altered mental status, P/F ratio of < 300, oliguria or serum creatinine >2.0, platelet count <100,000, INR >1.5. Meanwhile Grade II (moderate) is defined by any two of the following: Abnormal WBC count, febrile (≥39 °C), ≥75 years old, total bilirubin ≥5 mg/dL, hypoalbuminemia (<STD × 0.7). Grade I (mild) was defined as not meeting grade III or II criteria [4].
Since 2007, fluids, antibiotics, and analgesics have been the crux of management for ascending cholangitis. Biliary decompression has been used in severe or moderate cases of ascending cholangitis [4]. ERCP emerged as the first line step in decompression as it allows for interventions such as stone removal or stent placement; however, the optimal timing of performing an ERCP was not clear. Small observational studies found a delay in ERCP was associated with worse outcomes [3] and possibly length of stay [4].
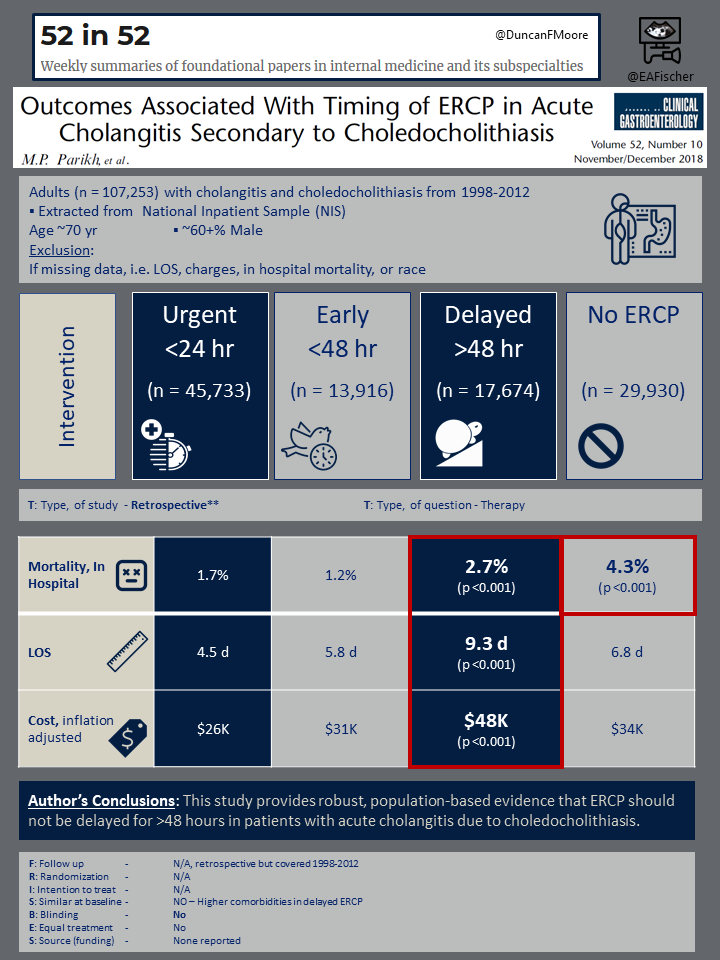
Parikh et al. sought to evaluate the optimal timing of ERCP in the management of cholangitis, with a larger cohort of patients. This study found that ERCP performed within 48 hours of presentation in patients with ascending cholangitis due to choledocholithiasis was associated with reduced mortality and length of stay.
Patient population
This study was performed as a population-based retrospective study using data from the national inpatient sample database. Only patients classified as cholangitis and choledocholithiasis were included. A total of 107,253 patient encounters were assessed. In addition, procedural codes were queried to identify if ERCP, percutaneous transluminal cholangiography, or other procedures were performed.
The majority of the patient population was white. Most patients had Medicare, followed by private insurance, and Medicaid. In terms of hospital size, the majority of the hospitals were in an urban location and were large (100-500+ beds); however, small (1-299 beds) and medium hospitals (50-499 beds) were included. The most common comorbidities were hypertension, electrolyte imbalances, anemia, coagulopathy, diabetes, pulmonary disease and heart failure.
Outcomes
The study was designed to evaluate the optimal timing for ERCP in ascending cholangitis due to choledocholithiasis with the primary outcome of mortality. Patients were grouped by if they underwent urgent (<24 hours), early (<48 hours), delayed (>48 hours) or no ERCP.
Important secondary outcomes were length of stay, hospitalization costs, and need for percutaneous transluminal cholangiography or related procedures.
Furthermore, a multivariable analysis was performed to adjust for age, race, comorbidities (via the Charleson Comorbidity Index), income, hospital size, location and teaching vs non-teaching hospitals. There were no major safety outcomes reported.
Results
Of the over 107,000 patients who fit into the inclusion criteria, over 77,000 patients underwent an ERCP. Most patients underwent an urgent ERCP (42.1%), followed by delayed ERCP (16.5%) and early ERCP (13%).
The majority of patients who underwent a delayed ERCP were older (72 years) (p < 0.001). Additionally, subjects in delayed ERCP group were more likely to have coagulopathy than no ERCP or urgent ERCP group. And in regards to comorbidities, patients in the delayed ERCP group (>48 h) were significantly more likely to have congestive heart failure, valvular heart disease, chronic pulmonary disease, neurological disorders, renal failure, fluid/electrolyte disorders, anemia, and a higher creatineine clearance. This is mirrored in the Charlson Comorbidity Index, which was highest in the delayed ERCP category (p < 0.001).
Mortality was highest in the no ERCP category and the delayed ERCP category (p <0.001). There was no statically significant difference in mortality among the patients who underwent early ERCP verses urgent ERCP. Multivariate analysis was performed adjusting for factors that could impact the the primary outcome, such as age, ethnicity, gender and Charlson Comorbidity index and the results were similar.
The length of stay was statistically significant in the delayed ERCP group for being longer than the other groups at 10 days (p <0.001). After adjusting for age, ethnicity, gender, Charlson Comorbidity index, hospital size and location, teaching versus non-teaching hospitals, the shortest length of stay was observed in the urgent ERCP group (5 days), followed by early ERCP group (6.2 days), and the no ERCP (6 days).
Similarly, the hospitalization cost was highest in the delayed ERCP group. The lowest cost was in the urgent ERCP group. Finally, percutaneous transluminal cholangiography (PTC) was generally being performed in the no ERCP group at 10.9%. In the delayed ERCP group, PTC and related procedures were required in 6.4%.
Discussion
This trial, though retrospective, paved the way in defining the optimal time frame for ERCP in acute cholangitis secondary to choledocholithiasis. Delays in ERCP were associated with worse outcomes including mortality, increased length of stay and increase in health care costs [1, 2]. However, the major limitation in interpreting the results are related to its retrospective nature. The delayed ERCP group was older with more comorbidities, factors, which by themselves could be associated with delays in any procedure and a worse outcome. That the multivariate adjustments did not affect the findings. A recent systematic review and meta-analysis, combining 7534 patients from 9 observational studies, showed that ERCP within 48 h of symptom onset was associated with a reduction in early and late mortality, organ failure, and length of hospitalization [5].
Although there may be multiple barriers to early ERCP (<48 hours) such as persistent hemodynamic instability or difficulties with access to specialized care in smaller hospitals, it is imperative that we as providers recognize the necessary interventions required to improve patient outcomes. Due to the robust evidence provided in this paper, and subsequent meta-analysis, ERCP within 48 hours of presentation of ascending cholangitis due to choledocholithiasis has become the standard of care.
Summary by Zaeema Zafar
| F: Follow up | N/A, retrospective |
| R: Randomization | N/A |
| I: Intention to treat | N/A |
| S: Similar at baseline | NO, delayed ERCP group older with more comorbidities |
| B: Blinding | No |
| E: Equal treatment | N/A |
| S: Source (funding) | Not discussed |
References
- Ohdan H, Oshiro H, Yamamoto Y, et al. Bacteriological investigation of bile in patients with cholelithiasis. Surg Today 1993; 23:390.
- Kiriyama S, Takada T, Strasberg SM, et al. Tokyo Guidelines Revision Committee. New diagnostic criteria and severity assessment of acute cholangitis in revised Tokyo Guidelines. J Hepatobiliary Pancreat Sci. 2012;19:548–556.
- Khashab MA, Tariq A, Tariq U, et al. Delayed and unsuccessful endoscopic retrograde cholangiopancreatography are associated with worse outcomes in patients with acute cholangitis. Clin Gastroenterol Hepatol. 2012;10:1157–1161.
- Parikh ND, Issaka R, Lapin B, et al. Inpatient weekend ERCP is associated with a reduction in patient length of stay. Am J Gastroenterol. 2014;109:465–470. Erratum in: Am J Gastroenterol 2014;109:616.
- Iqbal U, Khara HS, Hu Y, Khan MA, Ovalle A, Siddique O, Sun H, Shellenberger MJ. Emergent versus urgent ERCP in acute cholangitis: a systematic review and meta-analysis. Gastrointest Endosc. 2020 Apr;91(4):753-760.e4.
