Milan Criteria
Liver Transplantation for the Treatment of Small Hepatocellular Carcinomas in Patients with Cirrhosis.
Mazzaferro V, Regalia E, Doci R, et al.
N Engl J Med. 1996 Mar 14;334(11):693-9. [Full Text]
Summary by William Davis, DO
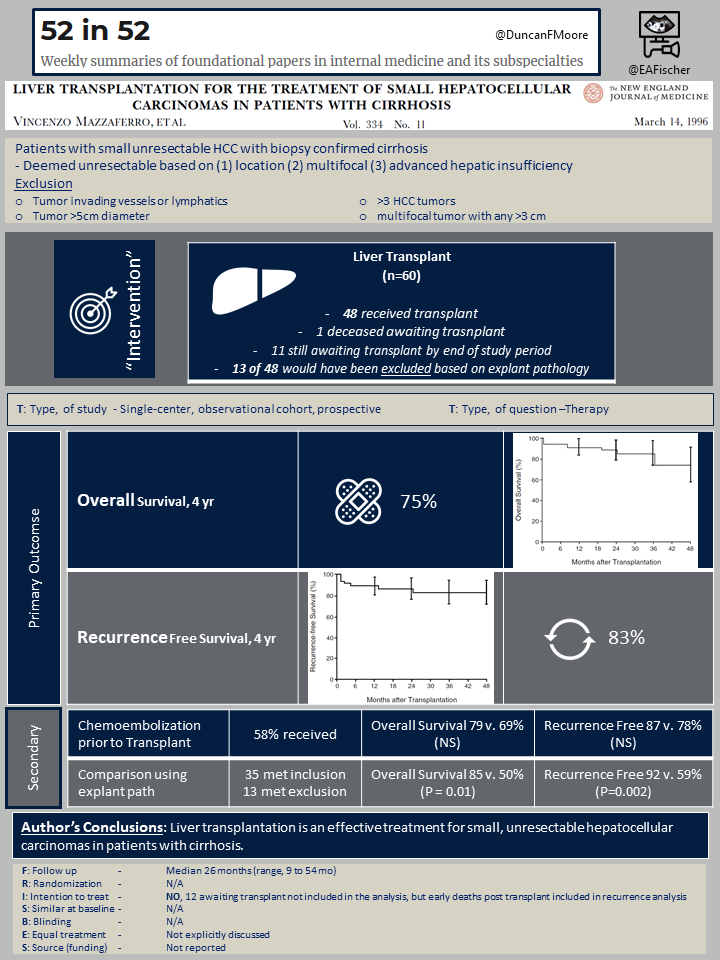
At the time of this study (1991-1995), liver transplant in the treatment of cirrhosis complicated by hepatocellular carcinoma (HCC) was controversial. It was difficult to determine which patients would have improved outcome. The yearly risk of HCC in with is 3% and HCC in cirrhosis portends a poor prognostic (3 year survival rate of 25%). This was a landmark study in demonstrating that some patients will benefit from liver transplant in the setting of HCC small nonresectable cirrhosis. Now 25 years later we continue to consider this studies inclusion criteria in selecting HCC patients for transplant; namely, one tumor measuring ≤5cm or ≤3 tumors measuring up to 3cm along with no vascular or extrahepatic involvement (the Milan Criteria).
Patient population
A total of 295 patients with hepatocellular carcinoma (HCC) were evaluated during the study period. Only 60 patients (20%) of this cohort had biopsy proven cirrhosis, meeting inclusion criteria. Of those, 94% had hepatitis B, hepatitis C or co-infection related cirrhosis. The remaining 6% had cirrhosis from: multifocal fibrolamellar HCC (n=1), attributed to alcoholic (n=1) or cryptogenic (n-1) cirrhosis. Of the 60 eligible patients, 48 received liver transplant. Twelve patients did not receive transplant. One patient died awaiting transplant and the other 11 patients were still waiting for transplant by end of study period.
Exclusion criteria:
- Non-cirrhotic HCC
- HCC was resectable
- HCC with Single tumor ≥5cm in diameter
- HCC with ≥3 tumors
- Multifocal HCC with either tumor >3 cm in diameter
- Tumor invasion of blood vessels
- Tumor invasion of lymph nodes
Outcomes
The primary outcome was overall and recurrence-free survival at 4 years.
Important secondary outcomes included if pre-transplant treatment with chemotherapy had a survival benefit. Chemotherapy was given to patients who were deemed to have hepatic sufficiency based of Childs Pugh score (CPS) Class A or B. When compared with CPS Class C who did not receive chemotherapy, there was no statistical difference in overall survival. An additional secondary outcome was the rate of recurrence of HCC in the transplanted liver.
Surveillance occurred every three months with ultrasonography, chest radiography, and measurement of serum alpha-fetoprotein in all patients; abdominal and thoracic computed tomographic (CT) scans were obtained every six months, and radionuclide bone scans were obtained every eight month.
Results
Survival was assessed with prospective following over a 4 year period with median follow up being 26 months. The studies primary outcome was overall survival. 4-year overall survival was 75% and recurrence-free survival was 83%.
This pathology of the explanted liver was reviewed to see if patients actually did meet inclusion criteria. Liver autopsy confirmed that 35 of 48 patients met inclusion criteria but 13 of 48 patients pathology would have actually been excluded. In 3 patients a higher grade HCC was identified on explanted liver pathology.
Recategorizing these groups found that the overall survival in the 35 patients still meeting inclusion compared to the 13 patients not meeting was 85% vs. 50% and recurrence free survival was 92% vs. 59% (both differences were significant, P=0.01 and P=0.002, respectively).
Secondary outcomes demonstrated that chemoembolization prior to liver transplant did affect the outcome. 58% of patients (CPS Calls A and B) received pre-treatment with chemoembolization with 4-year overall survival and recurrence-free survival was 79 and 87% respectively vs 69 and 78% in those that did not receive pre-transplant chemotherapy (CPS Class C). This did was not a statistical difference.
Rate of recurrence of HCC in transplanted liver occurred in 4 of 48 patients (8.33%).
Discussion
Once considered a controversial treatment for cirrhosis complicated by unresectable HCC, liver transplant seemed to prolong survival in this single-center prospective cohort. Of particular importance for predicting survival with transplantation in early HCC were other factors such as T stage, number of tumors, alpha fetal protein concentration or presence/absence of capsule were unreliable. The studies 4-year overall survival was 75% compared to a 3-year survival rate of 25% with no intervention.
The inclusion, or Milan criteria, demonstrated the importance of patient selection in HCC cirrhosis (1,2). As patients that met inclusion criteria on both pre-screening and on autopsy of explanted liver had significantly higher overall survival than transplanted patients who would have been excluded based on explanted liver autopsy findings (85% vs 50%).
Additionally, patient selection also showed significance in HCC recurrence. Of the 4 patients that demonstrated recurrence, 3 patients demonstrated higher tumor staging on explant liver pathology than assigned preoperatively. This further signifies the importance of Milan criteria in patient selection and overall prognosis post liver transplant.
Twenty years later this ground breaking study has paved the way to identify the patient population of HCC cirrhosis that will have a good prognosis after liver transplant.
Though the inclusion criteria over time has been expanded, the Milan Criteria continues to be the backbone (3). Additionally, despite no survival benefit found in pre-transplant therapy in the above study, bridging therapy continues to be used today in practice (1,4). Particularly, bridging therapy is recommended to hinder tumor progression for transplant listed patients with an estimated waiting period of ≥6 months (4). Typically this is achieved with locoregional therapies such as transarterial chemoembolization or radio frequency ablation (4).
References
- Meirelles Júnior RF erreir., Salvalaggio P, Rezende MB run. de, Evangelista AS, Guardia BD ell., Matielo CE duard. L, et al. Liver transplantation: history, outcomes and perspectives. Einstein (Sao Paulo). 2015;13(1):149–52.
- Grandhi MS, Kim AK, Ronnekleiv-Kelly SM, Kamel IR, Ghasebeh MA, Pawlik TM. Hepatocellular carcinoma: From diagnosis to treatment. Surg Oncol [Internet]. 2016;25(2):74–85. Available from: http://dx.doi.org/10.1016/j.suronc.2016.03.002
- Pavel M, Fuster J, Pavel M, Fuster J. Expansion of the hepatocellular carcinoma Milan criteria in liver transplantation : Future directions. 2018;24(32):3626–36.
- Kollmann D, Selzner N, Selzner M. Bridging to liver transplantation in HCC patients. 2017;863–71.
