SPLIT
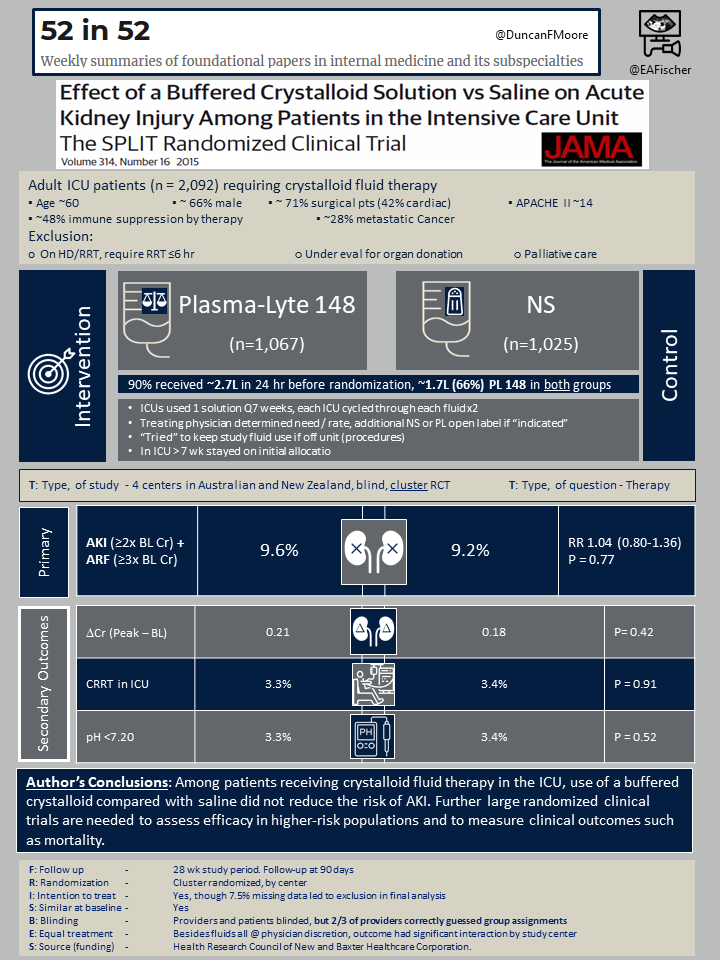
“Effect of a Buffered Crystalloid Solution vs Saline on Acute Kidney Injury Among Patients in the Intensive Care Unit: The SPLIT Randomized Clinical Trial.”
Young P, Bailey M, Beasley R, et al.; SPLIT Investigators
JAMA. 2015 Oct 27;314(16):1701-10. doi: 10.1001/jama.2015.12334. Erratum in: JAMA. 2015 Dec 15;314(23):2570. PMID: 26444692.
Those interested in the history of medicine may find “The history of 0.9% saline” an enjoyable read [1]. In it the authors note “the composition of 0.9% sodium chloride is dissimilar to most solutions used in the past, and is in no way ‘normal’ or ‘physiological’,” It seems was referred to as “normal” for being nearly isotonic.
The solution that was actually first referred to as “normal” saline was made as follows:
“3 drachms of chloride of sodium, 18 grains of chlorate of potash, 9 grains of phosphate of soda, and 60 grains of bicarbonate of soda, in 3 pints of distilled water”
It therefore contains 150 mEq Na, 128 mEq Cl, 2.5 mmol PO42, and 27 mEq HCO3[1, 2].
Non-physiologic is one thing. But clinical concerns have also been noted – use of normal saline (NS) is associated with acute kidney injury [3] and with mortality in critically ill septic patients [4]. It was in this setting that the SPLIT investigators designed their study.
SPLIT had a negative result and subsequently there has been better quality evidence favoring balanced crystalloids (i.e. SMART [5]). We will review SPLIT mainly as an exercise into evaluating what factors could have lead to a false negative result (type II error).
Population
A total of 2,092 adult ICU patients at 4 Australian / New Zealand centers that requiring crystalloid fluid therapy were recruited. The mean age was 60 years, most (66%) were male. There were more surgical (71%) than medical ICU patients (though 42% were cardiac. The group was relatively ill with APACHE II of 14.
The authors excluded those on HD/CRRT, that required CRRT ≤6 hr, anyone under evaluation for organ donation, or palliative only patients.
Study Design
The study was a blinded, cluster randomized trial. Each ICUs would only utilize wither Plasma-Lyte 148 (PL-148) or NS in 7 week increments. After 7 weeks the unit would change to exclusively the other solution for 7 weeks. Any patient in the ICU > 7 wk stayed on his/her initial allocation.
The treating physician determined need and rate of the fluid. The physician could also use additional NS or PL-148 in an open label fashion.
Outcomes
The primary outcome was the incidence of acute kidney injury (AKI), defined as an increase ≥2 times the baseline creatinine, or acute renal failure (ARF), defined as an increase ≥3 times the baseline creatinine.
Secondary outcomes included the need for CRRT, incidence of pH < 7.2 or the absolute creatinine change.
Results
A major observation was that in 24 hours before randomization 90% on patients had received >2 L of fluids and of that, about 1.7 L (66%) was PL-148, given to both groups.
There was no difference in the primary or secondary outcomes. The AKI+ARF rate was similar, 9.6% vs. 9.2% (RR 1.04, 95% CI 0.80-1.36, P = 0.77). The need for CRRT was infrequent and similar, 3.3% vs. 3.4% (p=0.91), and the incidence of pH < 7.2 or the absolute creatinine change were similar between groups.
Finally, on surveying the treating physicians, approximately 2/3 were able to guess the treatment assignment despite blinding.
Discussion
If this does represent a “false” negative finding, what factors could have contributed? Certainly if most physicians could guess the fluid in use although blinded this is a consideration.
More importantly, the event rate of AKI+ARF was relatively low, about 9%. In SMART the event rate was about 15% [5]. When a smaller event rate occurs within a smaller population (~2K pts SPLIT vs. ~7K pts SMART) it will be more difficult to detect a difference, even if there is one. The magnitude of the difference in SMART was not very large, which goes along with this.
Additionally, the run in period may have negated the effects of the intervention. Nearly the same amount of fluids were given before study enrollment (~2L) compared to within the intervention (~2.6L). That means both groups received a large portion of PL-148, the purpoted “safer” fluid.
As noted, though SMART results favor balanced cyrstalloids, the protection from AKI was not huge (OR 0.9, 95% CI 0.82-0.99). It may actually be the total volume infused that is the most important rather than type of fluid utilized. But regardless, one can see there are clear confounders in SPLIT that could have masked a true effect.
- Awad S, Allison SP, Lobo DN. The history of 0.9% saline. Clin Nutr. 2008 Apr;27(2):179-88. doi: 10.1016/j.clnu.2008.01.008. Epub 2008 Mar 3.
- Churton Dr. A case of scirrhus of the pylorus, with excessive vomiting; repeated intravenous injections of saline solution; remarks. Lancet, 132 (1888), pp. 620-621.
- Yunos NM, Bellomo R, Hegarty C, Story D, Ho L, Bailey M. Association between a chloride-liberal vs chloride-restrictive intravenous fluid administration strategy and kidney injury in critically ill adults. JAMA. 2012 Oct 17;308(15):1566-72.
- Raghunathan K, Shaw A, Nathanson B, Stürmer T, Brookhart A, Stefan MS, Setoguchi S, Beadles C, Lindenauer PK. Association between the choice of IV crystalloid and in-hospital mortality among critically ill adults with sepsis*. Crit Care Med. 2014 Jul;42(7):1585-91.
- Semler MW, Self WH, Wanderer JP, Ehrenfeld JM, Wang L, Byrne DW, Stollings JL, Kumar AB, Hughes CG, Hernandez A, Guillamondegui OD, May AK, Weavind L, Casey JD, Siew ED, Shaw AD, Bernard GR, Rice TW; SMART Investigators and the Pragmatic Critical Care Research Group. Balanced Crystalloids versus Saline in Critically Ill Adults. N Engl J Med. 2018 Mar 1;378(9):829-839.
