Risperdone or Haldol for Palliative Delirium
“Efficacy of Oral Risperidone, Haloperidol, or Placebo for Symptoms of Delirium Among Patients in Palliative Care: A Randomized Clinical Trial“
Agar MR, Lawlor PG, Quinn S, et al.
JAMA Intern Med. 2017;177(1):34–42. [Full text]
Delirium is a prevalent symptom in the hospital that many providers will see in their careers. It is estimated that 11-25% of elderly hospitalized patients have delirium upon admission, and an additional 29-31% will develop delirium their stay [1]. Previously providers were jumping straight to anti-psychotics for treatment; however, newer evidence suggests that this should not be the first-line treatment as it can lead to adverse outcomes. The following study aims to compare the results of the anti-psychotics Risperidone and Haloperidol with placebo in the treatment of delirium, specifically in inpatient palliative patients.
Design and Patient Population
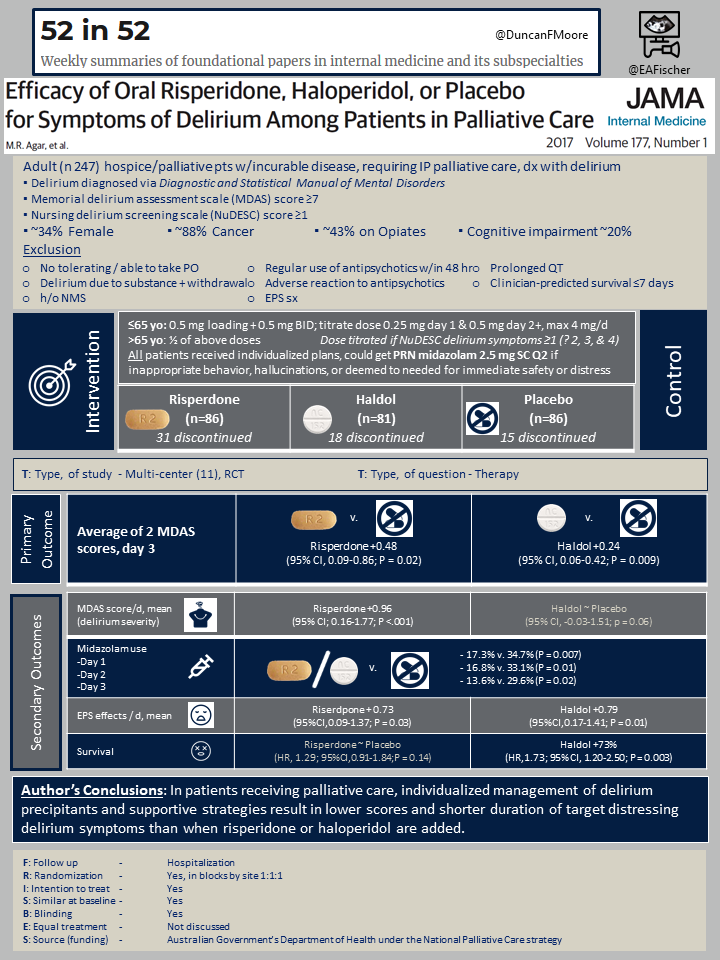
In order to be eligible, patients had to be at least 18 years, receiving hospice or palliative care with advanced disease that was incurable, and requiring inpatient palliative care. Patients also had to be able to swallow liquids. 306 patients were assessed for eligibility and 247 were included due to exclusion criteria or unwillingness to participate.
Patients were excluded if they had: delirium due to substance withdrawal, history of neuroleptic malignant syndrome, regular use of antipsychotics within 48 hours (could be included if only a 1-time dose > 24 hours prior to enrollment), adverse reaction to antipsychotics, extrapyramidal disorders, prolonged QT interval, clinician-predicted survival of 7 days or less, cerebrovascular accident or seizure in the past 30 days.
Outcomes
This study was a multi-site, double blind, placebo-controlled randomized clinical trial that took place in 11 inpatient hospice or palliative care services from August 13, 2008 to April 2, 2014 in Australia. Participants were randomized in a 1:1:1 ratio and both participants and researchers were blinded.
They were assigned to receive either oral Risperidone, Haloperidol, or placebo to help control delirium-induced behavior, communication, or hallucinations. Dosing of each drug was based on prior controlled trials and the dose was adjusted based on age. For example, adults older than 65 received half the starting dose than patients younger the 65. Of note, doses could also be titrated (up or down) during the study depending on the patient’s delirium score assessment which was conducted every 8 hours. Patients received their medication every 12 hours for a total of 72 hours. All patients also received individualized treatment plans, such that non-pharmacological causes of delirium were addressed.
- ≤65 yo: 0.5 mg loading + 0.5 mg BID; titrate dose 0.25 mg day 1 & 0.5 mg day 2+ to a max of 4 mg/d
- >65 yo: ½ of above doses
The primary outcome was to assess the change in delirium score (based on the nursing delirium screening scale NuDESC, with elements measuring inappropriate behavior, inappropriate communication, and illusions/hallucinations) between baseline to 72 hours.
The study also looked at the following secondary outcomes: delirium severity, midazolam use (the protocol outlined use of this medication for when participates scored high enough on the delirium assessment scale and were deemed to need immediate treatment for safety or distress), extrapyramidal effects, sedation, and survival.
Results
Both the Risperidone group and Haloperidol group had greater delirium symptom scores at study end than placebo (Risperidone group scores were 0.48 units higher than placebo (95% CI, 0.09-0.86; P = 0.02); Haloperidol group 0.24 units higher than placebo (95% CI, 0.06-0.42; P = 0.009). These results were statistically significant.
- Delirium severity: The Risperidone group scored higher on the MDAS score (delirium severity) per day as compared with the placebo (+0.96, 95% CI; 0.16-1.77; P <.001); the Haloperidol group didn’t reach statistical significance.
- Midazolam use: Midazolam was used less in the placebo arm as compared to the antipsychotic arms in each day of the study.
- Extrapyramidal effects: There were greater extrapyramidal effects in the antipsychotic arms as compared to the placebo arm for both Risperdone and Haloperidol.
- Sedation: There was no statistically significant difference in the Richmond Agitation Sedation score per day between Risperidone and placebo; however, there was a significant difference between scores when comparing the Haloperidol and placebo arms, such that the Haloperidol group scored higher.
- Survival: Of note 34 patients died during the study period. Those receiving Haloperidol were more likely to die as compared to placebo (HR,1.73; 95% CI, 1.20-2.50; P = 0.003). There was no statistical significance in survival rates when comparing Risperidone and placebo.
Discussion
From this data the author concluded that symptoms of delirium (as measured by behavior, communication, and perception) were greater in groups treated with anti-psychotics as compared to the placebo arm. Additionally, there was higher use of the rescue msidazolam as well as extrapyramidal side effects in the anti-psychotic arms compared to the placebo group. This suggests that supportive care and treating the underlying cause of delirium may reduce delirium more than the use of anti-psychotics and avoids potential adverse effects of those agents.
While the results should make us reconsider anti-psychotic use in palliatve delirium, there were limitations to note. First, patients were terminal and admitted for palliation, so these results may not be able to be extrapolated to other acutely-ill patients. Additionally, the majority of patients had mild to moderate delirium (based on the MDAS) at baseline. With severe delirium or in acute short term management we may still have to rely on anti-psychotics or benzodiazepines, especially if a safety concern arises, Lastly, the 3 day follow-up time may be too short for a condition that can last several days to even weeks, especially if a patient is deteriorating as many in the study did. The researchers did make note of the short follow-up time, but stated that if an intervention for delirium hadn’t worked within 72 hours they believed it was unlikely to benefit that patient.
We should always attempt to treating or ameliorate the underlying cause of delirium, such as infections, metabolic disturbances, medication toxicity, etc. In addition, trying to minimize deliriogenic environments by promoting sleep/wake cycles, minimizing interruptions, and frequently re-orientating patients, has benefit. Other work suggests that both trazodone monotherapy and the combination of trazodone and Ramelteon (drug mechanism similar to melatonin) can effectively manage delirium (with the latter having better results) [2]. Though it too has several limitations, it similarly suggests there are alternative agents to anti-psychotics for treating delirium.
- Vasilevskis EE, Han JH, Hughes CG, Ely EW. Epidemiology and risk factors for delirium across hospital settings. Best Pract Res Clin Anaesthesiol. 2012 Sep;26(3):277-87. doi: 10.1016/j.bpa.2012.07.003. PMID: 23040281; PMCID: PMC3580997
- Ishii T, Morimoto T, Shiraishi M, Kigawa Y, Narita K, et al. (2018) Retrospective Study of Trazodone Monotherapy Compared with Ramelteon and Trazodone Combination Therapy for the Management of Delirium. J Psychiatry 21: 444. doi:10.4172/2378-5756.100044
Summary by Alexis Thurmond
