ACCORD
“Effects of Intensive Glucose Lowering in Type 2 Diabetes”
by the Action to Control Cardiovascular Risk in Diabetes (ACCORD) Study Group
N Engl J Med. 2008 Jun 12;358(24):2545-59. [Free full text]
ACCORD goes back to 2008 and was landmark with many implications. It “established” that intensive blood glucose control can have significant consequences. But is it still applicable today?
Hypoglycemia certainly can have significant consequences. And in ACCORD the authors concluded “intensive therapy to target normal glycated hemoglobin levels for 3.5 years increased mortality and did not significantly reduce major cardiovascular events.” So what could be different in 2020?
PICO analysis is often taught as a way to design a literature search [1]. But it can also be used to put in context a study you have already selected to review. Additionally, the FRISBES heurisitc (Follow-up, Randomization, Intent-to-treat, Similar at baseline, Blinding, Equal treatment, Source of funding) allows for critical appraisal of that study [2, 3]. We will particularly look at the implications of the purposeful unequal treatment on the intensive target group.
“Unequal” treatment in ACCORD
By design ACCORD had unequal treatment between groups in order to achieve a lower A1C. Not surprisingly the Intensive group took more agents in combination. In fact 52+% in the Intensive group, compared to only 16-32% in the standard group were on 3 agents. And 10+% in the Intensive group vs. 1-2% were on 4-5 agents! How much of the worse outcome was just related to polypharmacy?
It is hard to know but we can look at what those agents were. Three of the agents are now effectively OBSOLETE, and one is off the market (Rosiglitazone) now in most of the world and rarely used in the US. 92% of the intensive group compared to only 58% of the standard group received a TZD (and 99% of those were Rosiglitazone – an agent associated with worse cardiovascular outcomes).
| Agent | Intensive | Standard | CV Associated AE |
| Insulin | 77% | 55% | Hypoglycemia, Weight gain |
| Metformin | 95% | 87% | – |
| Secretagogue | 87% | 74% | Hypoglycemia, Weight gain |
| TZDs (~99% Rosi) | 92% | 58% | ?MI, Weight Gain |
| α-Glucosidase inh | 23% | 5% | — |
A common theme of these older agents and insulin is weight GAIN. More insulin was needed to reach the target and insulin probably has the most associated weight gain of the agents listed. In fact, the intensive group had 28% gain >10 kg over the study period compared to only 14% in the standard group (P<0.001). Not surprisingly the intensive group also had more hygoglycemic events, with 10.5% vs 3.5% (P<0.001) of patients having events requiring medical assistance.
The authors did attempt to identify an association with the increased mortality (including Rosi use). While no individual cause could be identified, between polypharmacy, using agents with directly associated CV events (Rosi), and others with indirect CV effects (weight gain, hypoglycemia), one can see why the increased mortality is confounded and possibly not “from” the lower A1C target. Post HOC analysis of the patients even showed that the mortality within the intensive group was driven by patients with persistently high A1Cs, or patients that did not achieve the low target A1C [4].
Target A1C in 2020?
Back to the question about interpreting ACCORD in 2020? Modern agents (i.e. targeting DDP4 , SGLT2, GLP-1, etc.) have low or no association with hypoglycemia. Many are weight neutral or even have indications for weight loss, independent of diabetes. And finally are being shown to have multiple cardiovascular and renal protective effects (to be discussed in future 52in52s).
The actual ideal A1C target is somewhat controversial, but targeting a lower A1C may be reasonable in some patients. But at the least, extrapolating ACCORD in 2020 as low A1C = increased mortality is problematic. Not surprisingly, guideline A1C targets vary between the various endocrine, diabetic and general medicine societies [5] (because of this and many other nuanced interpretations of DM data over time).
Below you can find the original 52in52medicine methodologic summary of ACCORD by Duncan F. Moore, MD.
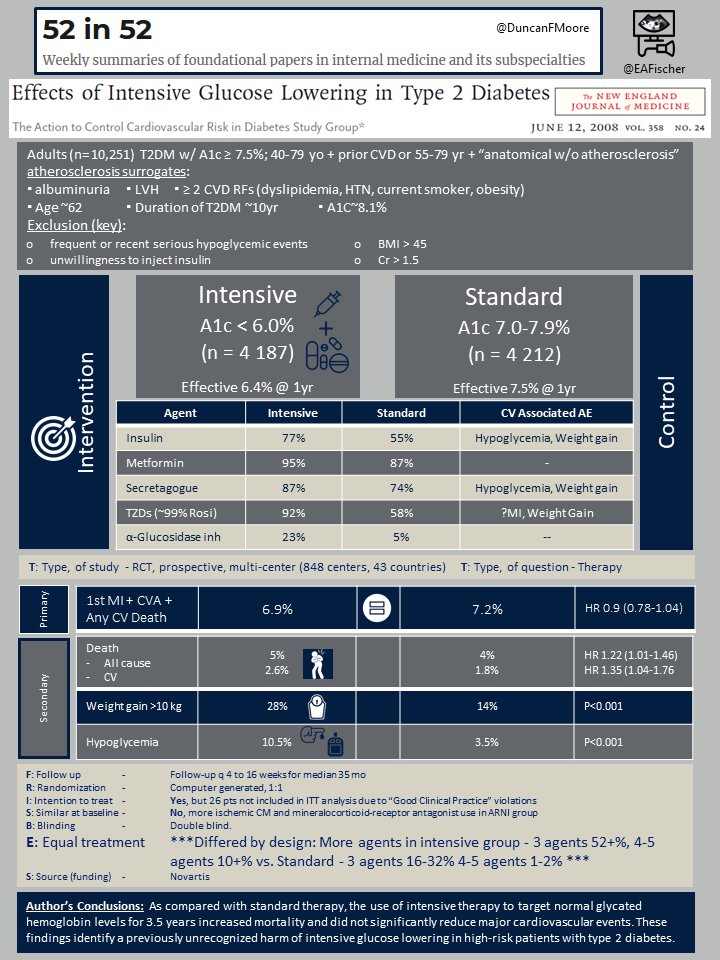
The trial enrolled patients with T2DM with A1c ≥ 7.5% and either age 40-79 with prior cardiovascular disease or age 55-79 with “anatomical evidence of significant atherosclerosis,” albuminuria, LVH, or ≥ 2 additional risk factors for cardiovascular disease (dyslipidemia, HTN, current smoker, or obesity). Notable exclusion criteria included “frequent or recent serious hypoglycemic events,” an unwillingness to inject insulin, BMI > 45, Cr > 1.5, or “other serious illness.” Patients were randomized to either intensive therapy targeting A1c to < 6.0% or to standard therapy targeting A1c 7.0-7.9%. The primary outcome was a composite first nonfatal MI or nonfatal stroke and death from cardiovascular causes. Reported secondary outcomes included all-cause mortality, severe hypoglycemia, heart failure, motor vehicle accidents in which the patient was the driver, fluid retention, and weight gain.
10,251 patients were randomized. The average age was 62, the average duration of T2DM was 10 years, and the average A1c was 8.1%. Both groups lowered their median A1c quickly, and median A1c values of the two groups separated rapidly within the first four months. (See Figure 1.) The intensive-therapy group had more exposure to antihyperglycemics of all classes. See Table 2.) Drugs were more frequently added, removed, or titrated in the intensive-therapy group (4.4 times per year versus 2.0 times per year in the standard-therapy group). At one year, the intensive-therapy group had a median A1c of 6.4% versus 7.5% in the standard-therapy group.
The primary outcome of MI/stroke/cardiovascular death occurred in 352 (6.9%) intensive-therapy patients versus 371 (7.2%) standard-therapy patients (HR 0.90, 95% CI 0.78-1.04, p = 0.16). The trial was stopped early at a mean follow-up of 3.5 years due to increased all-cause mortality in the intensive-therapy group. 257 (5.0%) of the intensive-therapy patients died, but only 203 (4.0%) of the standard-therapy patients died (HR 1.22, 95% CI 1.01-1.46, p = 0.04). For every 95 patients treated with intensive therapy for 3.5 years, one extra patient died. Death from cardiovascular causes was also increased in the intensive-therapy group (HR 1.35, 95% CI 1.04-1.76, p = 0.02). Regarding additional secondary outcomes, the intensive-therapy group had higher rates of hypoglycemia, weight gain, and fluid retention than the standard-therapy group. (See Table 3.) There were no group differences in rates of heart failure or motor vehicle accidents in which the patient was the driver.
Intensive glucose control of T2DM increased all-cause mortality and did not alter the risk of cardiovascular events. This harm was previously unrecognized. The authors performed sensitivities analyses, including non-prespecified analyses, such as group differences in use of drugs like rosiglitazone, and they were unable to find an explanation for this increased mortality.
- Schardt C, Adams MB, Owens T, Keitz S, Fontelo P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med Inform Decis Mak. 2007 Jun 15;7:16. doi: 10.1186/1472-6947-7-16.
- Lupi C, Lefevre F, Ward-Peterson M, 2017, ‘Evidence-based medicine skills that last: A transferable model utilizing integration, spaced learning, and repetition with a single study design among second-year medical students’, MedEdPublish, 6, [4], 52, https://doi.org/10.15694/mep.2017.000221
- Duke Teaching and Leading EBM. (2017). Duke Teaching and Leading EBM: A Workshop for Educators and Champions of Evidence-Based Medicine.
- Riddle MC, Ambrosius WT, Brillon DJ, Buse JB, Byington RP, Cohen RM, Goff DC Jr, Malozowski S, Margolis KL, Probstfield JL, Schnall A, Seaquist ER; Action to Control Cardiovascular Risk in Diabetes Investigators. Epidemiologic relationships between A1C and all-cause mortality during a median 3.4-year follow-up of glycemic treatment in the ACCORD trial. Diabetes Care. 2010 May;33(5):983-90. doi: 10.2337/dc09-1278.
- Smetana GW, Nathan DM, Dugdale DC, Burns RB. To What Target Hemoglobin A1c Level Would You Treat This Patient With Type 2 Diabetes?: Grand Rounds Discussion From Beth Israel Deaconess Medical Center. Ann Intern Med. 2019 Oct 1;171(7):505-513. doi: 10.7326/M19-0946.
