COMPLETE – Complete Multivessel PCI for MI
Complete Revascularization with Multivessel PCI for Myocardial Infarction
Mehta SR, Wood DA, Storey RF, et al.
N Engl J Med. 2019 Oct 10; 381:1411-21. [Full text]
Summary by Martin McNamara
For several decades primary percutaneous coronary intervention (PCI) has been the preferred reperfusion method for patients with acute ST-segment elevation myocardial infarction (STEMI). More than half of these patients are found to have multivessel coronary artery disease (CAD) in addition to the culprit lesion that caused the patient’s STEMI during the primary PCI [1]. It has been debated whether nonculprit, angiographically significant lesions found incidentally during primary PCI should be intervened upon. Observational studies have shown a possible benefit in reduced events with staged nonculprit-lesion PCI, but these studies were criticized for possible selection bias and confounding [2,3]. Meanwhile, randomized controlled trials up to this point had shown reductions in composite outcomes with nonculprit-lesion PCI; however, these trials were relatively small in size with results driven predominantly by the decreased risk of subsequent revascularization with that strategy [4-6]. Meta-analyses have also suggested a clinical benefit with nonculprit-lesion PCI, but when emphasizing concrete clinical endpoints such as reduction of death or MI, there was insufficient evidence to support nonculprit-lesion PCI or complete revascularization [7-9]. The COMPLETE trial, powered for these robust clinical end points, was designed to address this evidence gap.
Patient population and Design
All patients included in the study presented with STEMI, underwent PCI of the culprit lesion, and had evidence of angiographically significant, multivessel CAD. Eligible patients underwent randomization within 72 hours after successful primary PCI of the culprit lesion.
Multivessel CAD was defined as the presence of at least one angiographically significant non-infarct-related (nonculprit) lesion that was amenable to successful treatment with PCI and was located in a vessel with a diameter of at least 2.5 mm that was not stented as part of the index culprit-lesion PCI.
Nonculprit lesions were deemed angiographically significant if they were associated with at least 70% stenosis of the vessel diameter on visual estimation or with 50 to 69% stenosis accompanied by a fractional flow reserve (FFR) measurement of 0.80 or less.
The main exclusion criteria were an intention before randomization to revascularize a nonculprit lesion, a planned surgical revascularization, or previous CABG. Eligible subjects were randomized in a 1:1 fashion to receive either routine staged PCI of all suitable nonculprit lesions within 45 days after randomization or guideline based medical therapy with no further revascularization.
For the complete revascularization group, randomization was stratified according to the intended timing of nonculprit-lesion PCI either during or after index hospitalization. Guideline-based medical therapy was recommended in both treatment groups and included dual antiplatelet therapy with aspirin indefinitely and ticagrelor for at least one year (though one quarter of the patients received clopidogrel). High-dose statin therapy, angiotensin-converting-enzyme inhibitors or angiotensin-receptor blockers, mineralocorticoid-receptor antagonists, and beta-blockers were also recommended.
Results
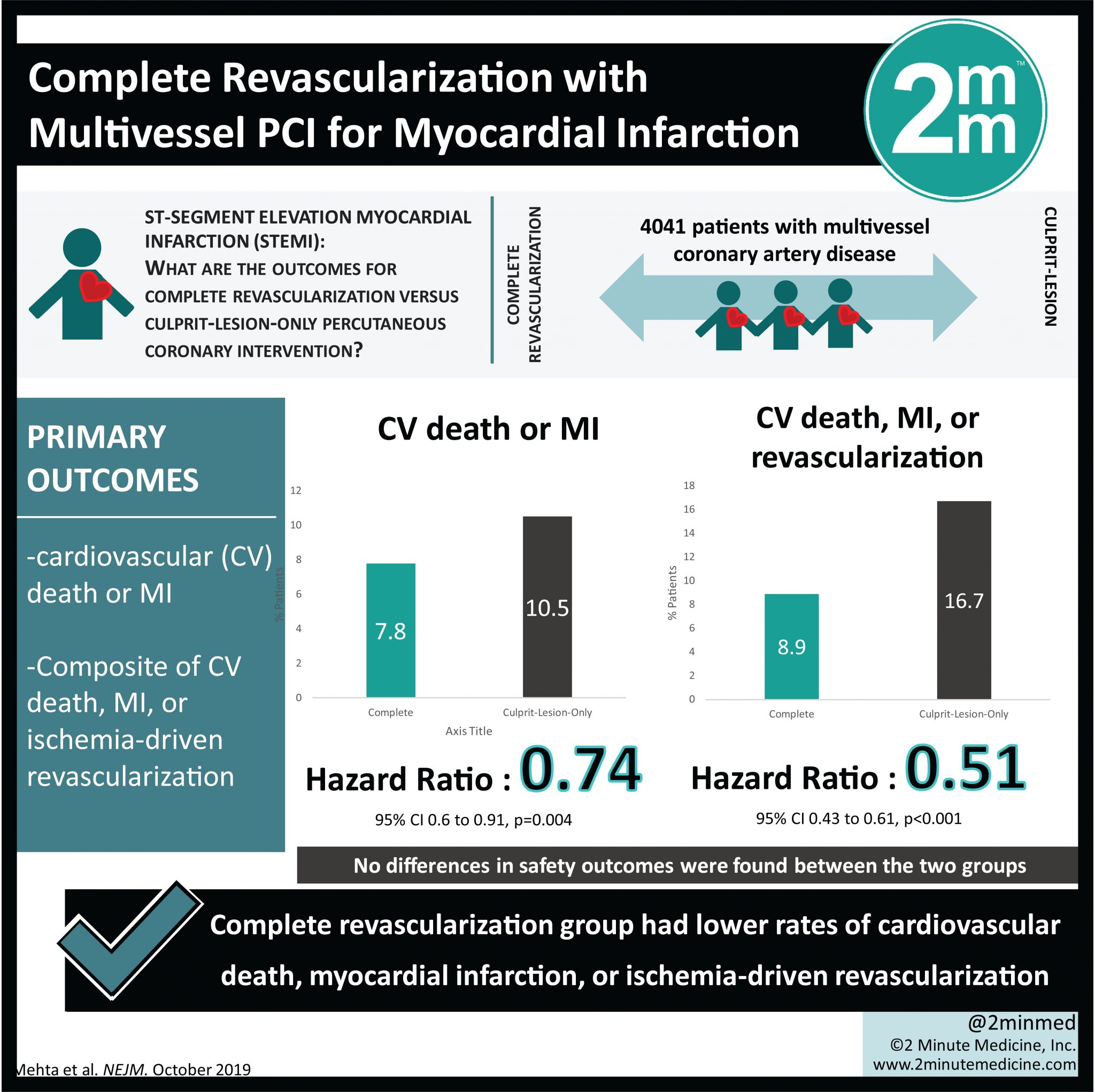
A total of 4041 patients were enrolled in the study between February 2013 and March 2017 from 140 centers in 31 different countries. 2016 patients were randomized to the complete revascularization group, and 2025 patients were randomized to the culprit lesion-only group. The median follow up was 3 years. Baseline characteristics between the two groups were the same.
The first coprimary outcome was the composite of cardiovascular death and new MI, which occurred in 158 patients in the complete-revascularization group versus 213 in the culprit-lesion-only PCI group (7.8% vs. 10.5%, p = 0.004; NNT 37). The second coprimary outcome was the composite of cardiovascular death, new MI, or ischemia driven revascularization, which occurred in 127 in the complete-revascularization group versus 339 in the culprit-lesion-only PCI group (8.9% vs. 16.7%, p < 0.001; NNT 13). For both primary outcomes, the benefit of complete revascularization was observed irrespective of timing. Regarding secondary and safety outcomes, there was no significant group difference in major bleeding, stroke, stent thrombosis, and contrast-associated acute kidney injury.
Discussion
The COMPLETE trial demonstrated that among patients with STEMI and multivessel CAD, complete revascularization of culprit and significant non-culprit lesions performed during the index hospitalization or soon after discharge is superior to culprit-lesion only PCI in reducing risk of cardiovascular death or myocardial infarction, as well as cardiovascular death, myocardial infarction, or ischemia-driven revascularization, without an increase in adverse events. Additionally, the benefit of such complete revascularization is apparent over the long term, as evident by continued divergence of the Kaplan–Meier curves for several years.
The “COMPLETE Timing Sub-study” was published shortly after and highlighted that the benefit of complete revascularization over culprit-lesion only PCI was consistent irrespective of the timing of staged nonculprit-lesion intervention [10]. Regardless of whether staged PCI of nonculprit lesions occurs during hospitalization or up to 45 days following STEMI, similar reductions in cardiovascular death, MI, and ischemia-driven revascularization were seen. Currently, there is no clear evidence favoring no-nculprit PCI during hospitalization over early after discharge in this patient population.
There are some limitations of the COMPLETE trial worth mentioning. First, non-culprit lesion PCI was not performed during the index culprit lesion PCI for STEMI, which will have to be further assessed in future trials. Also, no patients with cardiogenic shock were included, and in general the multivessel CAD complexity was low (as measured by the SYNTAX score). Extrapolating the practice to more ill or complex patients should be done with caution, In subgroup analysis, the benefit was limit to men, with non significance in women, though the study was not powered for this outcome.
Does COMPLETE change practice? Current guidelines suggest risk stratification of those with multivessel CAD, so some do potentially already undergo non-culprit PCI. The COMPLETE authors continue to follow these patients longer term. If the long term findings mirror these, it will likely be enough to change guidelines.
| F: Follow up | 3 years |
| R: Randomization | Yes |
| I: Intention to treat | Yes |
| S: Similar at baseline | Yes |
| B: Blinding | NO |
| E: Equal treatment | Yes |
| S: Source (funding) | Canadian Institutes of Health and Research, AstraZeneca, and Boston Scientific. |
- Park DW, Clare RM, Schulte PJ, et al. Extent, location, and clinical significance of non-infarct-related coronary artery disease among patients with ST-elevation myocardial infarction. JAMA 2014;312: 2019-27.
- Hannan EL, Samadashvili Z, Walford G, et al. Culprit vessel percutaneous coronary intervention versus multivessel and staged percutaneous coronary intervention for ST-segment elevation myocardial infarction patients with multivessel disease. JACC Cardiovasc Interv 2010;3:22-31
- Bainey KR, Mehta SR, Lai T, Welsh RC. Complete vs culprit-only revascularization for patients with multivessel disease undergoing primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: a systematic review and meta-analysis. American heart journal 2014;167:1-14.e2.
- Wald DS, Morris JK, Wald NJ, et al. Randomized trial of preventive angioplasty in myocardial infarction. The New England journal of medicine 2013;369:1115-23.
- Gershlick AH, Khan JN, Kelly DJ, et al. Randomized trial of complete versus lesion-only revascularization in patients undergoing primary percutaneous coronary intervention for STEMI and multivessel disease: the CvLPRIT trial. Journal of the American College of Cardiology 2015;65:963-72.
- Engstrøm T, Kelbæk H, Helqvist S, et al. Complete revascularisation versus treatment of the culprit lesion only in patients with ST-segment elevation myocardial infarction and multivessel disease (DANAMI-3—PRIMULTI): an open-label, randomised controlled trial. Lancet (London, England) 2015;386:665-71.
- Bainey KR, Welsh RC, Toklu B, Bangalore S. Complete vs Culprit-Only Percutaneous Coronary Intervention in STEMI With Multivessel Disease: A Meta-analysis and Trial Sequential Analysis of Randomized Trials. Can J Cardiol 2016;32:1542-51
- Elgendy IY, Mahmoud AN, Kumbhani DJ, Bhatt DL, Bavry AA. Complete or Culprit-Only Revascularization for Patients With Multivessel Coronary Artery Disease Undergoing Percutaneous Coronary Intervention: A Pairwise and Network Meta-Analysis of Randomized Trials. JACC Cardiovasc Interv 2017;10:315-24.
- Tarantini G, D’Amico G, Brener SJ, et al. Survival After Varying Revascularization Strategies in Patients With ST-Segment Elevation Myocardial Infarction and Multivessel Coronary Artery Disease: A Pairwise and Network Meta-Analysis. JACC Cardiovasc Interv 2016;9:1765-76.
- Wood DA, Cairns JA, Wang J, et al. Timing of Staged Nonculprit Artery Revascularization in Patients With ST-Segment Elevation Myocardial Infarction: COMPLETE Trial. Journal of the American College of Cardiology 2019;74:2713-23.
- O’Gara PT, Kushner FG, Ascheim DD, et al.; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Jan 29;127(4):e362-425. doi: 10.1161/CIR.0b013e3182742cf6. Epub 2012 Dec 17.